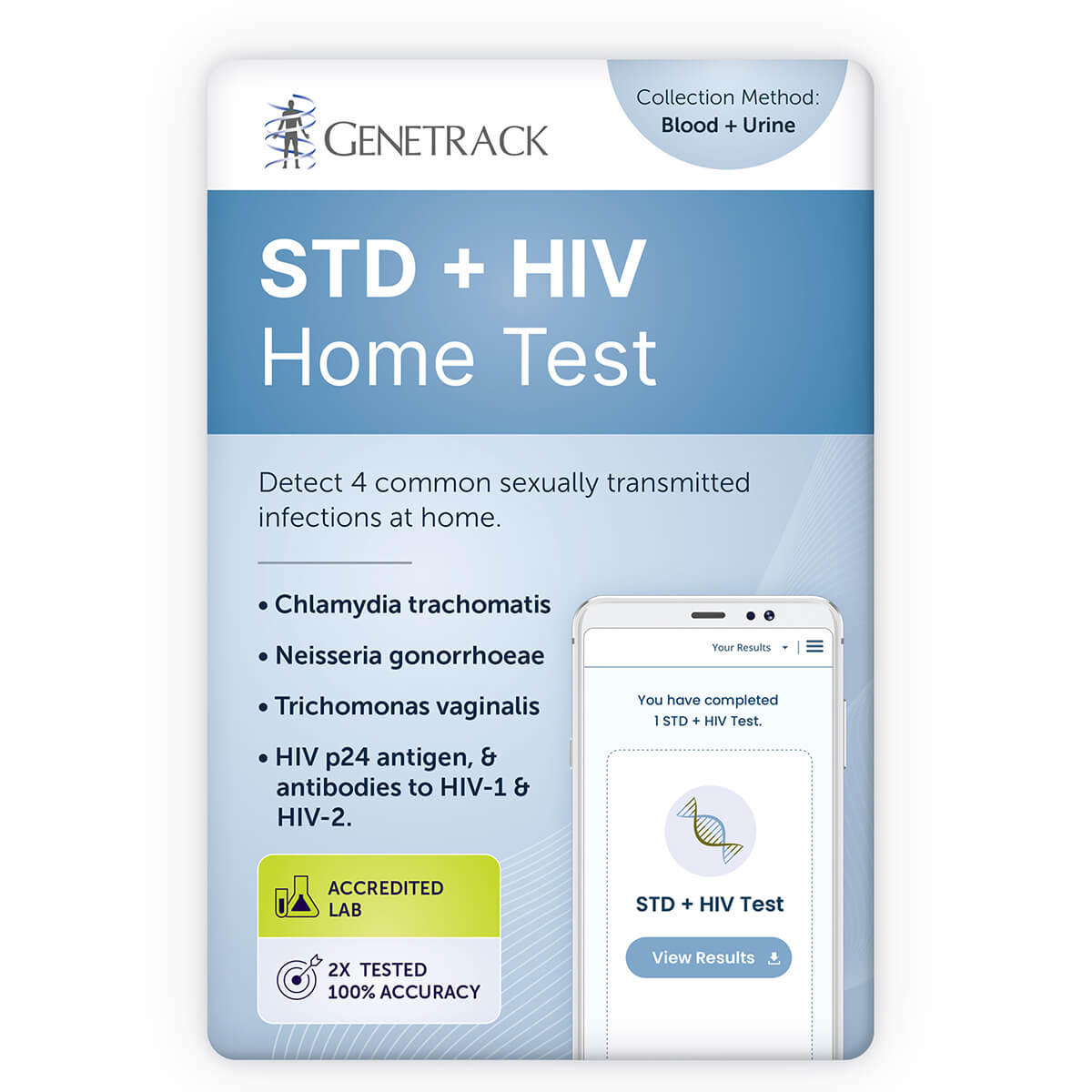
STD+HIV Test
Detection of Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis by nucleic acid amplification technology.
Detection of the HIV p24 antigen, and antibodies to HIV-1 and HIV-2 by chemiluminescent microparticle immunoassay.
$119.00
Details
What is Included?
Sexually transmitted diseases (STDs) are also known as sexually transmitted infections (STIs). They are infections that are usually spread from person to person during vaginal, anal, and oral sex. Although many STDs are quite common, a lot of infected people do not show any symptoms, and are unaware that they have an STD and can pass the disease to others. Without treatment, STDs can lead to serious health complications. However, most STDs are easy to test for and can be effectively treated.
Chlamydia, gonorrhea and trichomoniasis:
Chlamydia, gonorrhea and trichomoniasis are common sexually transmitted diseases (STDs) caused by Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis. Both men and women can be infected; however, many infected individuals do not show any symptoms. Early detection enables prompt treatment to prevent transmission and long-term health complications, such as pelvic inflammatory disease and infertility.
HIV:
HIV is often a silent infection in the early stages with no obvious symptoms. However, this initial stage of acute HIV infection is when HIV is the most infectious. Prompt and accurate diagnosis is essential to begin antiretroviral therapy immediately to prevent the transmission of HIV.
Turnaround Time
1 – 3 business days
The turnaround time is not guaranteed. The average turnaround time is 1 – 3 business days from the date that the sample arrives at the laboratory. Shipping time for the sample is not included. Additional time is required if the case requires confirmatory or reflex testing, or if the sample is insufficient, or if a recollection is required.
Related Documents
- Patient Brochure
- Physician Brochure
- Sample Report
Additional Information and Resources
- » The importance of STD tests
- » I just had unsafe sex. Should I take an STD test immediately?
- » I tested positive for an STD. Should my partner get tested too?
- » What are the symptoms of some of the common STDs?
- » Will using condoms prevent me catching an STD?
- » How common are STDs?
- » Are STDs during pregnancy dangerous?
- » Why does it hurt to pee?
SPECIMEN REQUIREMENTS
Preparation Before Specimen Collection
- Do not urinate for at least one hour prior to urine collection.
- Females should not cleanse the labial area prior to urine collection.
- For individuals receiving anticoagulants, collect specimen prior to heparin therapy.
Specimen Type
First-void urine
Urine sample collected from the initial urine stream at least one hour after previous urination.
Blood
Blood sample collected from a finger prick.
Volume
Urine: 2 mL from a 20 – 30 mL collection of first-void urine.
Repeat urine collection (at least 1 hour after previous urination) if more than 60ml of first-void urine is collected.
Blood: Dried blood spot collection onto 5 circles on the collection card or 50 μL in a microtainer.
Container
Urine: Urine specimen transport container
Blood: Blood collection card or microtainer (regular blood tube)
Collection Method
This test requires a first-void urine specimen and a blood sample from a finger prick.
Urine:
Wait at least 1 hour after previous urination before collecting the first-void urine. All supplies for sample collection are provided in this kit.
- Collect 20 – 30 mL from the initial urine stream into the sterile urine collection container. Collection of larger volumes of urine may result in specimen dilution that may reduce test sensitivity; lesser volumes may not adequately rinse organisms into the specimen.
- Transfer 2 mL of urine into the urine specimen transport container using the disposable pipette provided. Transfer to the urine specimen transport container must occur within 24 hours of collection, and liquid level must fall between the two black indicator lines on the tube label.
- Re-cap the urine specimen transport container tightly. Seal in the transport bag and return to the laboratory in the provided prepaid return-shipping envelope.
Blood:
- First wash and dry hands. Warm hands aid in blood collection.
- Clean the finger prick site with the alcohol swab and allow to air dry.
- Use the provided lancet to puncture the skin in one quick, continuous and deliberate stroke.
- Wipe away the first drop of blood.
- Massage hand and finger to increase blood flow to the puncture site. Angle arm and hand downwards to facilitate blood collection on the fingertip.
- Drip blood onto the blood collection card or into the microtainer tube.
- Dispose of all sharps safely and return sample to the laboratory in the provided prepaid return shipping envelope.
NOTES: Avoid squeezing or ‘milking’ the finger excessively. If more blood is required and blood flow stops, perform a second skin puncture on another finger. Do not touch the fingertip.
Specimen Storage
Maintain specimen at temperatures between 2°C and 30°C during storage and transport.
Specimen Stability
Urine specimens stored at temperatures between 2°C and 30°C must be tested within 30 days of collection. If longer storage is required, urine specimens may be frozen in the urine specimen transport container within 7 days of collection and tested within 12 month of collection.
Dried blood spots can be refrigerated or kept at room temperature for up to 30 days. Blood samples can be refrigerated or kept at room temperature for up to 7 days.
Causes for Rejection
- Incorrect or incomplete patient identification
- Incorrect specimen collection
- Inappropriate storage and transport conditions
- Loss of urine specimen through container leakage
- Incorrect specimen volume
- Specimen received >30 days after collection
TEST DETAILS
Purpose
To detect Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis nucleic acid in a urine specimen
To detect HIV antigen and/or antibodies in a blood sample for screening for HIV infections. Supplementary tests are required for confirmation of positive results in this assay.
To detect Treponema pallidum antibodies in a blood sample for screening for syphilis infections. Supplementary tests are required for confirmation of reactive results in this assay.
Limitations
- This report is not intended for use in medico-legal applications.
- These results are intended for screening and monitoring for chlamydia, gonorrhea, and trichomoniasis and should be interpreted in conjunction with other laboratory and clinical information.
- Correct specimen collection and handling is required for optimal assay performance.
- The effects of tampon use, douching, and specimen collection variables have not been assessed for their impact on the detection of chlamydia, gonorrhea, and trichomoniasis.
- A negative result does not exclude the possibility of infection. False-negative test results may occur due to improper specimen collection, concurrent antibiotic therapy, presence of inhibitors, or organism levels below the sensitivity of this assay.
- A false-negative test result for syphilis may occur in severely immunosuppressed people (e.g., AIDS patients).
- False-positive results are rare, but may be more frequent in low-prevalence populations. A false-positive result may also occur directly after successful antimicrobial therapy, as Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis nucleic acids may persist for 3 weeks or more. For this reason, this test cannot be used for determining therapeutic success or failure.
- Female urine specimens may detect up to 10% fewer infections when compared with vaginal and endocervical swab specimens.
- False results may occur in specimens from individuals that have received preparations of mouse monoclonal antibodies for diagnosis or therapy. Additional clinical or diagnostic information may be required for these specimens.
- Assay interference may occur in specimens from individuals routinely exposed to animals or to animal serum products. Additional clinical or diagnostic information may be required for these specimens.
Methodology
Nucleic acid amplifications:
Chlamydia trachomatis
Neisseria gonorrhoeae
Trichomonas vaginalis
Chemiluminescent microparticle immunoassays:
Alinity i HIV Ag/Ab Combo
Alinity i Syphilis TP assay